

About
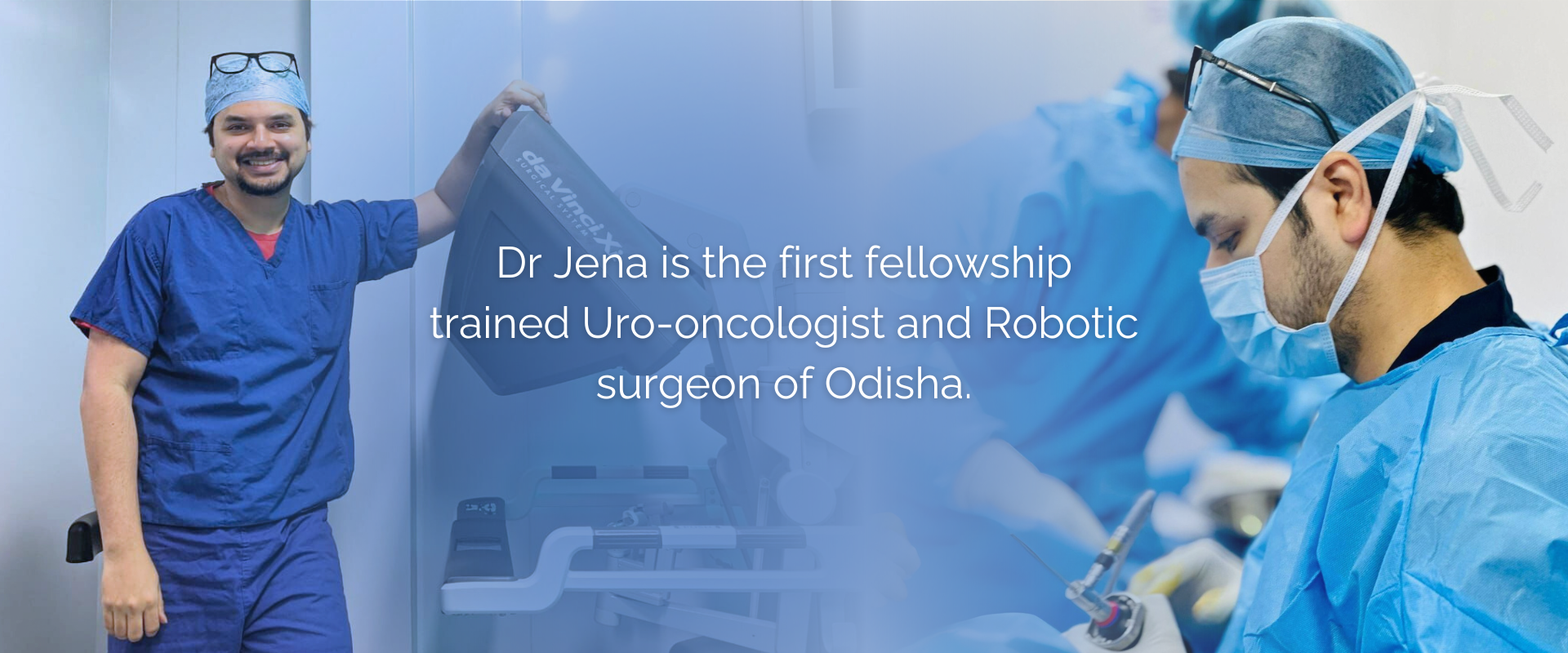
Dr Rahul Jena is a Consultant Uro-oncologist and Robotic surgeon at the Bagchi Sri Shankara Cancer Centre and Research Institute at Bhubaneswar, Odisha. The Bagchi Sri Shankara Cancer Centre is a state of the art, 750 bedded comprehensive cancer centre located in the upcoming Info valley area in Bhubaneswar and Dr Jena is the lead consultant for Uro-oncology services. Dr Jena is the first fellowship trained Uro-oncologist and Robotic surgeon of Odisha. He has had a stellar academic career.
Degrees
Educational Degrees
- M.B.B.S. (Hons)(AFMC, Pune),
- M.S. (General Surgery, PGIMER, Chandigarh)
- M.Ch. (Urology, SGPGIMS, Lucknow)
- Post Doctoral Fellow – Uro-oncology (SGPGIMS, Lucknow)
- Former Assistant Professor, Department of Urology, AIIMS, Jodhpur
- Senior Clinical Fellow in Robotic pelvic oncology & Uro-oncology, The Royal Marsden Hospital NHS Trust, Chelsea, London
- Consultant Uro-oncologist, Bagchi Shri Shankara Cancer Center and Research Institute, Bhubaneswar
Experience

Conditions Treated
Prostate Cancer

PROSTATE CANCER
Prostate cancer is one of the most common malignancies affecting the elderly male. Almost 1 in 10 males would be affected by it in their lifetime. It generally affects males after the age of 50 years but men with a family history of prostate cancer can be affected even at a much younger age. Recent research has shown that the number of men developing prostate cancer during their lifetime is going to increase. Diagnosing this cancer at its initial stages is of extreme importance, like in any other cancer, but more so in prostate cancer as it provides a window for complete cure from this cancer and normal life expectancy following radical therapy for early stages. Most of these cancers are asymptomatic to begin with in their earlier stages. However, the common presenting symptoms with which patients come to us are new onset difficulty in passing urine, poor urinary stream, frequent urination, blood in urine, urinary retention and back aches or bony pains, the latter seen in advanced and metastatic stages of the disease. A simple blood test called the Prostate Specific Antigen test can indicate whether the patient has prostate cancer or not and this can be confirmed with a histopathological examination, also known as the biopsy of the prostate. A MRI and a PSMA PET scan also helps in picking up this cancer and in staging the disease. Treatment depends on the stage of the disease. Early prostate cancer can be completely cured either by surgery or radiotherapy. However it is important to understand which is best for whom. Surgery involves complete removal of the prostate and its surrounding structures along with the nearby lymph nodes. The surgery can be done robotically, laparoscopically or by open means. All 3 approaches have equal outcomes in terms of cancer free state. But the robotic and laparoscopic approaches involve a shorter hospital stay and less pain. Most of the patients would be completely treated with surgery alone and would not require any additional therapy apart from a regular follow up with Serum PSA levels. Patients with locally advanced disease may require additional hormone and radiation therapy after the surgical removal of the prostate depending upon the final histopathology report. Chemotherapy drugs are used to kill cancer cells or stop them from growing. While not typically the first-line treatment for prostate cancer, chemotherapy may be used when the cancer has spread beyond the prostate gland and is no longer responding to hormone therapy. Immunotherapy works by stimulating the body’s immune system to recognize and attack cancer cells. Drugs known as checkpoint inhibitors, such as pembrolizumab and ipilimumab, have shown promise in treating advanced prostate cancer in some patients. Targeted therapy drugs are designed to specifically target molecules or pathways involved in cancer growth and spread. For example, drugs that target the androgen receptor pathway, such as enzalutamide and abiraterone, are used to treat advanced prostate cancer that has become resistant to hormone therapy. Alongside cancer-directed treatments, supportive care plays a crucial role in managing prostate cancer. This includes managing symptoms such as pain, providing psychological support, and addressing side effects of treatment to improve the patient’s quality of life. Participation in clinical trials may offer access to innovative treatments and contribute to advancements in prostate cancer management. These trials test new drugs, treatment combinations, or techniques to improve outcomes for patients with prostate cancer. The management of prostate cancer is evolving rapidly with ongoing research and advancements in treatment modalities. A personalized approach that considers the unique characteristics of each patient’s cancer is essential for achieving the best possible outcomes. Regular follow-up and monitoring are also important to detect any signs of recurrence or progression early and adjust treatment as needed.
Bladder Cancer

BLADDER CANCER
Bladder cancer is a type of cancer that begins in the cells of the bladder, the organ that stores urine. It’s one of the most common cancers, affecting both men and women, but it’s more common in men. There are several types of bladder cancer, but the most common type is transitional cell carcinoma, which begins in the cells that line the inside of the bladder.The exact cause of bladder cancer isn’t always clear, but some risk factors include smoking, exposure to certain chemicals, chronic bladder inflammation, and a family history of bladder cancer. Symptoms of bladder cancer may include blood in the urine, frequent urination, pain during urination, and lower back pain. Treatment for bladder cancer depends on the stage and type of cancer but may include surgery, chemotherapy, radiation therapy, immunotherapy, or a combination of these treatments. Early detection and treatment are crucial for improving outcomes and prognosis. Advanced metastatic disease may present with bony pains, cough, breathlessness and blood in sputum. Initial diagnosis is made with the help of a Ultrasound scan which can be easily done nowadays. Confirmation of the size and location of the tumor is done with the help of a dedicated CT scan. What follows next is an endoscopic surgery called Trans Urethral Resection of Bladder Tumor (TURBT) which removes all of the tumor from the bladder and provides tissue for histopathological examination and biopsy, which establishes the type, grade and stage of tumor. This surgery is done under anaesthesia and is done through the natural orifice of urine, and does not require any cuts or incisions. Patients are generally sent home one to two days after the surgery. Further treatment depends on the stage of the disease as determined by the biopsy report. A PET scan is done (for muscle invasive disease) to assess if there are any distant metastases or if the tumor is just localized to the bladder. Initial stages, which is the non muscle invasive stage, require instillation of BCG or a chemotherapeutic agent in the bladder along with cystoscopic surveillance. This intravesical therapy prevents the tumor from recurring and progressing. The drug is initially instilled weekly for 6 weeks, which is the induction course, followed by monthly instillations, which is the maintenance regimen. The more advanced stage, which is the muscle invasive, stage requires a radical surgery which involves removal of the whole bladder, besides the prostate in the males and uterus, cervix and fallopian tubes in females. The bladder is replaced by a replica bladder made from the intestines called a neobladder or a loop to facilitate collection of urine outside the body called an ileal conduit. The gold standard for bladder removal has always been a surgery called a radical cystectomy, but sometimes bladder preservation is also possible for advanced bladder cancers. Patients not fit for anaesthesia and surgery are offered radiotherapy and chemotherapy with a curative intent. Follow up after surgery involves regular visits to your doctor for physical examination, routine blood tests and a cross sectional imaging such as a CT scan. Patients with metastatic disease are treated with systemic chemotherapy and immunotherapy. Treatment plans are often individualized based on the patient’s specific situation, and multidisciplinary teams consisting of urologists, medical oncologists, radiation oncologists, and other specialists work together to determine the most appropriate treatment approach. It’s essential for patients to discuss their treatment options thoroughly with their healthcare team to make informed decisions about their care.
Kidney Cancer

KIDNEY CANCER
Kidney cancers arise in patients generally aged beyond 60, both in males and females and commonly present with blood in urine, pain in abdomen, or a lump in abdomen which is seen in more advanced stages. However about 60 % of the patients diagnosed with renal cancer are asymptomatic, and detected to have the lesion on an abdominal ultrasound done for an unrelated reason. The major risk factor for development of renal cancer is tobacco exposure, mainly in the form of smoking. The risk almost doubles with every 10 years of smoking. Other risk factors include obesity, hypertension, chronic NSAID painkiller use and some industrial chemical exposure. Kidney tumours are diagnosed and characterised by abdominal CT scans. The mainstay of treatment of these tumours are surgical removal, either removal of the whole kidney, known as radical nephrectomy, or just removal of the tumour while preserving the rest of the kidney in the case of small masses, known as partial nephrectomy. Kidney tumours do not respond to radiotherapy or chemotherapy and they should never be used as first line treatment options. Minimally invasive approach in the form of robotic surgery or laparoscopic surgery is the preferred form of surgery and avoids the morbidity of a large incision of an open surgery. Patients with metastatic and advanced disease are treated with targeted therapy with Tyrosine Kinase inhibitors or with the newer immunotherapeutic agents.
Testicular Cancer

TESTICULAR CANCER
Testicular cancer usually presents with painless enlargement of the testis. Most patients notice it on their own while in the shower. Attention is drawn towards an enlarging testes usually after a trivial trauma. There is an associated decrease in sensation of the afflicted testes. The age of presentation, prognosis and treatment modalities differ for these two types of tumor. Distinction amongst these two types of tumor is made initially by the blood levels of Alpha feto protein (AFP), Beta Human Chorionic Gonadotropin (B-HCG) levels and Lactate dehydrogenase (LDH) levels. The first step of treatment is to do a procedure called a high inguinal orchiectomy whereby the affected testes is removed through an incision in the groin. Scrotal orchiectomy or biopsy before removal of the testes should never be done. Final diagnosis is made by histopathological examination. Staging is done using CT scans of the chest and the abdomen to detect spread to the abdominal nodes. Treatment depends on the stage of the disease and the type of tumor (Seminoma vs Non Seminoma) and levels of blood markers. Initial stages are managed with high inguinal orchidectomy followed by surveillance while the more advanced stages need chemotherapy and surgery (Retroperitoneal Lymph Node Dissection (RPLND)) or radiotherapy depending upon the tumor subtype. RPLND can be done using open, laparoscopic or robotic approach. It is important to understand that testicular cancer has excellent cure rates if detected and treated early and appropriately.
Penile Cancer

PENILE CANCER
Penile cancer presents with a growth, usually involving the head or the foreskin of the penis. Uncircumcised males with poor hygiene are at high risk of developing a lesion, and circumcision is protective against penile cancers. The Human Papilloma Virus, responsible for cervical cancers in females, are also a causative factor for development of penile cancer. A warty growth on the glans is the most common presentation, while earlier stages might present with discolouration or a patch on the glans and the more advanced stages present with a cauliflower like growth replacing a part or the whole of the penis. Some patients also have swelling and ulcers in the inguinal region on one or both sides at presentation, representing more advanced stages of the disease. Diagnosis is based on clinical examination and a CT scan of the chest, abdomen and pelvis to detect metastases. A wedge biopsy of the lesion confirms the diagnosis and the final treatment depends on the stage of the disease. Smaller lesions can be treated with partial excision of the glans or partial amputation of the penis. Larger growths require a radical penectomy or removal of the whole penis and creation of perineal urethrostomy. Most of the patients also require a bilateral inguinal and pelvic lymph node dissection which is done by open approach or a minimally invasive approach called VEIL (Video Endoscopic Inguinal Lymphadenectomy). VEIL can be done laparoscopically or robotically and has added benefits over open surgery. Larger inoperable tumors can be treated with radiotherapy and metastatic disease is treated with systemic cytotoxic chemotherapy.
Adrenal Cancer

ADRENAL CANCER
Adrenal tumours can either be benign tumors, adrenal cortical cancers or paraganglioma arising from the adrenal medulla known as pheochromocytomas. Tumors arising from the cortex of the adrenal, whether benign or adrenal cortical carcinoma, are usually asymptomatic, but may present with abdominal pain or a lump in cases of large masses. Some of these tumors also produce excess steroids and sex hormones and patients may present with symptoms arising from these excess production of the hormones. Patients with pheochromocytomas present with symptoms of catecholamine excess, the classical triad being headache, palpitation and excessive sweating. Hypertension and deranged glucose metabolism also results for excess production of catecholamine. Diagnosis is made based on CT scan of the abdomen and measurement of plasma metanephrine and nor metanephrine levels. Surgery is the mainstay of treatment for adrenal masses, for both cortical tumors and of pheochromocytomas, albeit pheochromocytomas require medical counteraction of the effects of excessive catecholamine before surgery. Robotic and laparoscopic approach provide a minimally invasive means of removal of the tumor with minimal morbidity as against an open approach.
Adv. Laparoscopic Urology

ADVANCED LAPAROSCOPIC UROLOGY
Advanced laparoscopy is transforming urology, offering minimally invasive surgery for complex conditions. Tiny incisions house a camera and surgical tools, allowing magnified visualization and precise procedures. Patients benefit from faster recovery, less pain, and improved cosmetic outcomes.
This technique tackles various urological concerns, including kidney and adrenal tumors, ureteropelvic junction obstruction, and prostate cancer. Advanced laparoscopy even incorporates robotic assistance for enhanced dexterity and control. While minimally invasive, it requires specialized training and expertise. Talk to your urologist to see if advanced laparoscopy is right for you.
Robotic Surgery

ENDOUROLOGY
GENERAL UROLOGY
Robotic urology refers to the application of robotic technology in the field of urology, which focuses on the diagnosis and treatment of diseases related to the male and female urinary tract and the male reproductive organs. Robotic systems, such as the da Vinci Surgical System, have revolutionized urological surgeries by offering enhanced precision, dexterity, and visualization to surgeons.
In robotic urology, procedures like prostatectomy (removal of the prostate gland), nephrectomy (removal of a kidney), cystectomy (removal of the bladder), pyeloplasty (surgery to correct a blockage in the ureteropelvic junction), and even reconstructive surgeries are performed using robotic assistance. The surgeon controls robotic arms equipped with surgical instruments and a camera from a console, allowing for minimally invasive surgery with smaller incisions, reduced blood loss, shorter hospital stays, and faster recovery times compared to traditional open surgery.
Robotic urology has become increasingly popular due to its benefits for both patients and surgeons, offering improved outcomes and a higher quality of care for various urological conditions.
Understanding the procedure with Dr. Rahul Jena
This short video introduces the patient care approach and explains the steps of the procedure in plain language — great to reassure new patients.
Research Papers
Dr Rahul Jena is a prolific researcher and has researched extensively in cancers of the prostate, urinary bladder, kidneys, testes, penis and adrenal glands and has close to 50 peer reviewed publications in national and international journals and multiple book chapters to his credit. He continues to envision and head multiple clinical trials.

Rahul Jena
❯ Google Scholar Profile
- BOOK Chapter: Jena, R., Choudhary, G.R. (2023). Management. In: Singh, P., Nayak, B., Panaiyadiyan, S. (eds) A Guide to Management of Urological Cancers. Springer, Singapore.
- Jena R, Bhargava P, Tripathi S, Taywade S, Yadav T, Sandhu AS, Singh M, Navriya SC, Bhirud DP, Aggarwal A, Choudhary GR. 18F‐fluoro‐2‐deoxy‐2‐d‐glucose PET‐CT (FDG PET‐CT) in staging of high‐risk renal and urothelial bladder cancers (COPPER‐T) trial protocol. BJUI Compass. 2023.
- Jena R, Issa R, Perry M. Radical cystectomy vs trimodality therapy for muscle-invasive bladder cancer: further extensive evaluation needed. The Lancet Oncology. 2023 Aug 1;24(8):e324.
- Jena R*, Shrivastava N, Sharma AP, Choudhary GR, Srivastava A. The Adequacy of Pelvic Lymphadenectomy During Radical Cystectomy for Carcinoma Urinary Bladder: A Narrative Review of Literature. Frontiers in Surgery. 2021 Jun 17;8:203.
Why Dr. Rahul Jena is the Best Urologist Doctor in Bhubaneswar?
If you are searching for the best urologist in Bhubaneswar, you should visit Dr. Rahul Jena. With years of experience and expertise in the field of Urooncology, Dr. Jena is a leading urology specialist in Bhubaneswar, known for his compassionate care and excellent surgical skills.
Dr. Jena is board-certified and has undergone extensive training in uro-oncology, making him a highly sought-after specialist in the field. He is dedicated to providing the highest quality of care to his patients and takes a personalized approach to each case, ensuring that every individual receives the best possible treatment plan tailored to their specific needs.
Dr. Rahul Jena is renowned as the best urologist doctor in Bhubaneswar, providing top-notch care for all urological concerns. With extensive expertise in treating kidney stones, prostate issues, urinary infections, and other urological disorders, he is a trusted name in the field. As a leading urology doctor in Bhubaneswar, Dr. Jena combines advanced medical techniques with a compassionate approach to ensure optimal patient outcomes. His clinic is equipped with cutting-edge technology, offering personalized treatment plans tailored to individual needs. If you’re seeking the best urologist in Bhubaneswar, Dr. Rahul Jena is your go-to specialist for comprehensive and reliable urological care. Schedule your consultation today!
PRIZES AND AWARDS

CKP Menon Prize for Best Paperfor “Obstructive Index – A Novel predictor of failure of conservative management in cases of antenatally detected unilateral pelvi-ureteric junction obstruction – A retro spective analysis” at USICON 2019 from 25th – 28th January, 2019 at Bubaneshwar, Odisha

CMC Ludhiana Prize for Best Poster for “Radical Cystectomy and W-shaped ileal orthotopic neobladder reconstruction with serosa-lined tunneled ureteroileal anastomoses: A critical analysis of short-term voiding patterns and urodynamic and functional outcomes.”held at the NZUSICON 2018 held at Ludhiana, Punjab In November 2018.

2nd Prize in NZUSI got Talent award session at NZUSICON 2022 – The annual conference of the North Zone chapter of the Urological Society of India, held at Bikaner from 29-31st October 2022.

2nd prize in moderated poster session at NZUSICON 2022 – The annual conference of the North Zone chapter of the Urological Society of India, held at Bikaner from 29-31st October 2022.
Expert Recommendations

Mr Omer Karim
From the first day we met, Rahul left a lasting impression with his dedication and academic knowledge. He is an extremely hard-working individual who always had the patient's best interest at heart. He was well liked by all members of the clinical and academic staff.

Dr. Gautam Ram Choudhury
I have known Dr. Rahul Jena since 2012 when he was a new trainee in General Surgery at PGIMER, Chandigarh. Even as a general surgery trainee, his knowledge and aptitude for urology impressed us all. His kindness and devotion towards his patients were striking. He joined me a colleague in the Department of Urology at All India Institute of Medical Sciences, Jodhpur and spent 3 years working with us. He was knowledgeable, devoted and hardworking and has a particular aptitude for training of residents and trainees. He is a capable surgeon and was a dependable colleague in tense and critical situations in the operation theater and outside.

Dr. Uday Pratap Singh
My association with Dr Jena goes back to 2016. He spent almost 5 years working with us in the Department of Urology and Renal Transplant at Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow. He initially joined as a Senior Resident in Urology and then later stayed on with us a Post Doctoral fellow in Uro-oncology. During his time with us he came across as a hard-working, devoted and compassionate doctor.
Google Reviews
EXCELLENTTrustindex verifies that the original source of the review is Google. Excellent behavior to patient more loving like his s.p d.r father his treatment and post care is best amongst infinity needs no bound I pray to God for his prosperity and serve also needy patients in equally his family will be blessed by sathya sai baba.. Sai ram🙏Posted onTrustindex verifies that the original source of the review is Google. Dr, Rahul Jena sir not only a best doctor but also a good human beingPosted onTrustindex verifies that the original source of the review is Google. I'm extremely grateful to Dr. Rahul Jena. He is incredibly knowledgeable and took the time to explain everything thoroughly. I felt very comfortable and reassured during my mother's consultation with him. He is not only an Excellent Doctor , he is simple, superb Human being, Sober, approachable, a friendly approach with smiling face with his selfless service . The best ever doctor I have met in my life . I highly recommend Dr. Rahul Jena for his expertise and caring approach.Posted onTrustindex verifies that the original source of the review is Google. A Second Opinion That Changed Everything When we first received the diagnosis of a malignant neoplasm in the kidney, we were overwhelmed. Multiple doctors had bluntly suggested a radical nephrectomy, essentially removing the entire kidney. At just 46 years old, that seemed drastic and heartbreaking. That’s when we found Dr. Rahul Jena — and it completely changed the course of our journey. From the very first consultation, Dr. Jena stood out not just for his exceptional credentials (trained in top institutions and a specialist in robotic pelvic oncology), but for his clarity, patience, and deep empathy. Unlike others who rushed us into extreme procedures, Dr. Jena took a step back, reviewed everything, and explained that a laparoscopic partial nephrectomy was still possible. He prioritized preserving as much of the kidney as he could, given the early age and long-term quality of life considerations. Patient-Centric Care at Its Best: What truly amazed us was the level of patience and attention Dr. Jena offered. I came in with 58 questions—yes, 58!—ranging from risks and success rates to how he would manage complications during surgery. Not once did he show frustration or try to cut the conversation short. Instead, he answered each one with clarity and kindness, helping us feel fully informed and reassured. He also discussed in detail about imaging—like the CT angio and delayed scans to assess drainage in both kidneys—and coordinated smoothly with other consultants like Dr. Sanjeeb for pre-anesthesia checkups. His holistic, multidisciplinary approach made us feel we were in the best hands. Dr. Jena successfully performed the laparoscopic partial nephrectomy, despite indicating in advance that there were high chances of conversion to radical due to complexity. Thankfully, he stayed true to his commitment and managed to preserve the kidney. This level of surgical skill, especially in uro-oncology and robotics, is not easy to find in our region. But his involvement didn’t stop at the operation. What touched us deeply was that he personally followed up multiple times after surgery. He checked in without us having to call, just to ensure the patient was healing well and felt comfortable. That kind of dedication is rare and speaks volumes about the kind of doctor—and person—he is. In today’s world, where medical care can often feel transactional and rushed, Dr. Rahul Jena is a rare gem. He is not only a brilliant uro-oncologist and surgeon, but also a deeply compassionate human being. His combination of expertise, honesty, empathy, and commitment makes him someone I would recommend without hesitation to anyone facing urological cancers. If you’re in doubt or scared, do yourself a favor and seek an opinion from Dr. Jena. He gave us hope, saved a kidney, and did it all while making us feel completely seen and supported. I am forever grateful.Posted onTrustindex verifies that the original source of the review is Google. I am highly impressed by his Treatment skills. He is very kind, gentle and caring Person. The way he explains everything about the disease and it's treatment procedure, along with the confidence in his words, truly makes you feel safe. He is Amazingly comfortable with patients of all ages and brings the same level of comfort to them during their most difficult times. I am living proof of his unwavering dedication to both his work and his patients. He came to the OPD to attend to my parent’s case, even while managing his own medical situation within his family. Thank You for making my Family feel Safe. Jay Jagannath🙏Posted onTrustindex verifies that the original source of the review is Google. Very good, excellent sabu kam heba sir 👏 tama pain. You are The BEST 👌 for ever ❤️.Posted onTrustindex verifies that the original source of the review is Google. Highly experienced and a good doctor who explain everything before treating patients.
Appointments
Dr Rahul Jena is a Consultant Urologist and Robotic surgeon at the Bagchi Sri Shankara Cancer Centre and Research Institute at Bhubaneshwar, Odisha.






